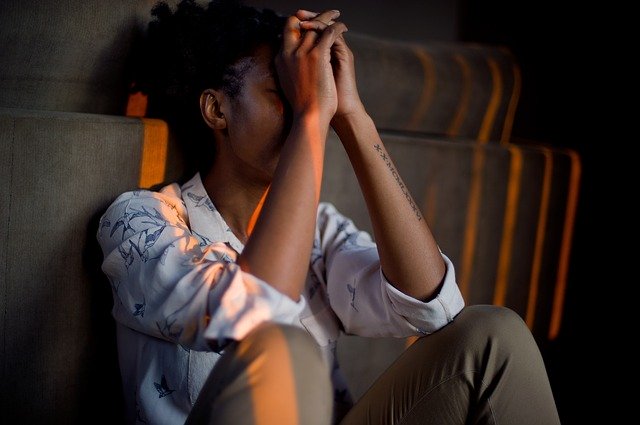
The Student Mental Health Epidemic
Depression and Anxiety on the University Campus
Read a summary using the INOMICS AI tool
In recent years, an epidemic has enveloped university campuses across the world - and it's not the COVID-19 coronavirus pandemic. Compared to any other generation of college students in history, current students experience more mental health issues than ever before. Some reports suggest that 35% of freshers in American universities experience anxiety disorders - and this percentage is compounded by the fact that, terrifyingly, nearly 10% of students have considered suicide in the previous twelve months. Since the 1950s, rates of suicides on American campuses have tripled, and it’s now the second most common cause of death among students. In the United Kingdom alone, a student commits suicide every four days.
Scarier than all this, though, is the real truth: that it’s not just college students, but all young people. Vindication for this comes from the conclusions of a psychiatric report from 2008 which found young people of student age but who don’t attend college to be equally as likely to suffer from some kind of psychiatric disorder as their college-going counterparts. Non-college attending individuals were more likely to self-medicate with drugs, whereas college students were at a higher risk of having some kind of alcohol misuse disorder. Among the initial sample of over 43,000 respondents, nearly one-half met the criteria for a psychiatric disorder. It’s glaringly obvious there’s a mental health crisis among young people. But why?
Money, drugs, and TLC
The reasons for this crisis are manifold and complex. The aforementioned 2008 study found that among both young adults of college-going age and the general population as a whole, loss of social support was a heavily contributing element in an increase in risk for psychiatric disorders. Another obvious explanation specific to university-goers could be the pressures students are put under to study long and hard and perform well, troubles mirrored among the non-student population in job insecurity, financial worries and the stress of the 9 to 5. Students are expected to deal not only with their studies, but also the stresses of moving away from home, living somewhere new, being thrust into a community of total strangers, and managing their own finances, all similar worries for young people attempting to purchase their first property and find a decent job. Moreover, n places like the United Kingdom and America, university fees are preposterously high, meaning many students live under financial strain and work part-time jobs – another pressure.
But these aren’t the only factors. Said stresses have changed little over time; half a century ago, students were still under pressure to perform well in their exams in an unfamiliar, potentially lonely environment. The financial burden was perhaps less, but – and without taking away its obvious impact – this can’t be used to explain the huge increase in disorders. One potential factor is the opening up of the conversation around mental health: students are more willing to talk about their struggles, so levels of diagnosis are higher, and therefore it appears there is an epidemic. But even this doesn't explain away the numbers. Even taking into account potential disparities in statistics, university campuses across the world are nonetheless experiencing a proportional upsurge in students who need help.
Perhaps the most important factor which has bee neglected is lifestyle. The stress of university can affect sleeping patterns, and getting enough sleep has been shown to be essential in staving off depression. Many students eat poorly, don’t exercise as much as they should, and often drink copious amounts, whether due to the university lifestyle in general or as a coping mechanism. Some experiment with drugs, which can become a crux, and a large number of students report feeling isolated and alone. Those who have difficulty making friends may be disproportionately affected. All of these are important contributing factors to mental illnesses. Recent studies from, among others, Dr Steve Ilardi, have shown, for example, that Omega-3 is a critical fatty acid in combating depression, and having a stable social circle and frequent social contact can work wonders. Being stuck inside all day studying at the computer doesn’t help either, as getting enough sunlight is an often-overlooked contributor to mental health difficulties.
Dr Ilardi recommends a programme which involves regular exercise, a tight-knit social circle, adequate Omega-3 and sufficient sleep every night. The trials have a 90% success rate (success being judged on patients not going into remission after 12 month). However, his programme potentially difficult to implement when one considers the stresses - and pressures - of university life. Universities themselves have a responsibility to deal with this problem, not just students. Unfortunately, these institutions are totally unprepared to deal with the problem.
System failure
The quality and crucially the availability of mental health care varies from university to university - but in general, it is inadequate. A survey at the University of California, San Francisco, suggested that of the 24% of students who were depressed, only 22% used mental health counselling services. Three of the main reasons students gave for not using services were cost at 28%, lack of confidentiality at 37%, and at the top of the list a lack of time, with nearly half – 48% – of students giving it as a reason not to attend. These results suggest not only that the mental health care systems in place aren't affordable for regular students, but also that the university system itself, at a foundational level, doesn't encourage either open dialogue nor space for students to look after their mental health.
This space needs to open up immediately, though. The discourse around mental health – specifically, the stigma that still surrounds it – is changing, but not fast enough. A study from 2009 in Medical Care Research and Review conducted on American campuses found that how students felt they were judged by their peers did not play a significant role in whether or not they sought help; their own personal feelings towards themselves were far more important. And these personal feelings of guilt, shame, whatever they may be, which caused people to close themselves off and feel uncomfortable talking about their mental health, were highly dependent on identity. Certain groups were far more at risk of stigmatising themselves than others: namely, younger, Asian, international, and/or more religious men, and predominantly those from poorer families. In the United Kingdom, men are just as likely to be depressed as women, but far less likely to seek help, and a far worse statistic highlights this point: suicide is the biggest killer of men under the age of 45, and men account for three-quarters of suicides in the United Kingdom. These stats will only get worse - and certain people will suffer more than others - if these spaces on campuses don't open up for this dialogue to take place.
Chemical solutions
Put in these terms, the problem seems insurmountable; fixing our youth is going to require time, money, and compassion on the behalf of the government, the health care system and universities, as well as us rethinking the way we want to live our lives. Fortunately, some are trying to come up with solutions before the university level. In New York, the Mental Health Association has launched an online training program to ‘help educators better prepare in supporting student mental health’. The program aims to aid teachers in their understanding of the signs and symptoms of mental health, as well as how it can affect youth development. New York State enacted a law in 2018 that made some form of mental health education mandatory in schools. Head over to India, and the same conversation is opening up, with positive effects. In Mangaluru, the District Mental Health team has begun organising camps to create awareness among teachers and parents of mental health issues, and has implemented a hotline system which students can call if they need counselling. Dr Ratnakar of the District Mental Health team says ‘the primary objective of the mission is to unearth the fear that is instilled in... young minds’ – in other words, to remove the stigma surrounding mental illness. These types of programs are especially effective as they try to mitigate the problem at an early age – during the school year. There is always the risk, however, that these types of top-down impositions can be crudely structured and organised, of low quality, even. Regardless, it’s a step in the right direction.
At the university level, there are necessary steps to be taken to mitigate the fallout of this epidemic. Universities should be promoting lifestyles that foster both physical and mental health, the two going hand in hand as they do. This means providing adequate facilities for both free and low-cost sports, as well as doing things like not allowing students to stay in the library all night in order to encourage healthy sleeping habits. Moreover, an environment in which talking about mental health is encouraged should be a priority. Aside from this, universities must work with healthcare providers to ensure counselling and support led by trained professionals are available for students whenever they need it. This would shorten waiting lists and guarantee the correct therapeutic route for the person in need. Equally as important, these services need to be properly publicised. Too often, student support services aren’t advertised to students, meaning they don’t take advantage of the services which could help them through their studies and, in more serious cases, save their life. This is especially true for emergency services for those close to mental breakdown or contemplating taking their own life – these services are essential and cannot be spared.
There’s a more serious issue that needs to be tackled if we are are to mitigate this problem, and it comes back to Dr Ilardi’s research. The modern lifestyle – as he puts it, our ‘sedentary, indoor, sleep-deprived, socially-isolated, fast-food-laden, frenetic’ modern life – is one conducive to mental illnesses, particularly depression. If we want to decrease the likelihood that people will experience mental illness, this needs to change. This isn’t just about providing healthcare and talking therapy for students; it’s about a fundamental shift in the way we interact with the world around us, the things we do to our bodies, and the way we live our lives. Until we do this, until we make this central structural change, rates of depression will continue to climb, irrespective of how many psychologists are available for weekly sit downs and how destigmatised the conversation becomes. The problem goes deeper than just discourse: it reaches right down into our bodies, the food we put in them, the people we interact with; in other words, into our very chemistry.
If you’re affected by mental illness or psychiatric problems, whatever they may be, it’s essential to talk to a GP or a mental health professional. If you're contemplating suicide, most countries have a suicide help line. The UK number for Samaritans is 116 123 and the US National Suicide Prevention Lifeline is 1-800-273-8255.
-
- PhD Program
- Posted 2 weeks ago
Graduate Program in Economics and Finance (GPEF) - Fully funded Ph.D. Positions
Starts 1 Sep at University of St.Gallen in Sankt Gallen, Switzerland
-
- Postdoc Job
- Posted 1 week ago
Postdoctoral Research Fellow Opportunity
At University of Notre Dame in Notre Dame, United States
-
- PhD Candidate Job
- Posted 2 weeks ago
3 PhD positions at the Vienna Graduate School of Economics (VGSE)
At Vienna Graduate School of Economics - VGSE in Vienna, Austria